Thursday, March 1, 2018, 11pm, I lay in bed trying not to panic. My heart was racing so fast I could not find my pulse. It was also erratic, jumping around like a kicking mule. At the same time, it felt like someone was sitting on my chest. I was home alone, waiting for Jim to return from his hockey game. ‘Breathe’ I repeated to myself. Relax.
When Jim arrived home and came to check on me, letting me know he was safely back from his West Island Game, I told him what was happening. ‘I’ll lay down with you and rub your back’, he suggested. I declined instead suggesting he take me to emergency. Convinced I was having a heart attack, the 20-minute ride from the house to Glengarry Memorial was torturous. Parking directly in front of the entrance, Jim ran inside to shout at the staff that I was having a heart attack as I slowly made my way inside. As I reflect back now, a bit of a comedy as he probably should have waited for me. Panic makes you crazy. I was admitted immediately, fortunately a quiet night in the ER. This was my first episode of Atrial Fibrillation (afib), one that took an additional 12 hours to resolve. I was sent by ambulance to Cornwall where the diagnosis was confirmed.
Four months later, during my second knee replacement surgery, I experienced my second major episode and spent the night in the recovery room instead of the comfort of a hospital room. Seven plus years later, as is usual with this condition, my afib episodes continue, increasing in frequency and duration. These episodes occur randomly with no identifiable triggers. They interrupt my sleep as they often occur at night, cause fatigue and of course, anxiety.
Over the course of my diagnosis, I have seen three specialists, two of them cardiologists. The standard Canadian approach to afib is to treat with anti-coagulants and beta blockers and take a “watch and wait” approach before offering the patient a ‘cardiac ablation’, a procedure which blocks the faulty wiring that causes afib. What this approach fails to account for is the effect the condition has on quality of life, the anxiety it causes, especially if you are travelling and leading an otherwise active lifestyle, and the risk of developing chronic afib, where your heart is in a constant state of arrythmia and/or congestive heart failure.
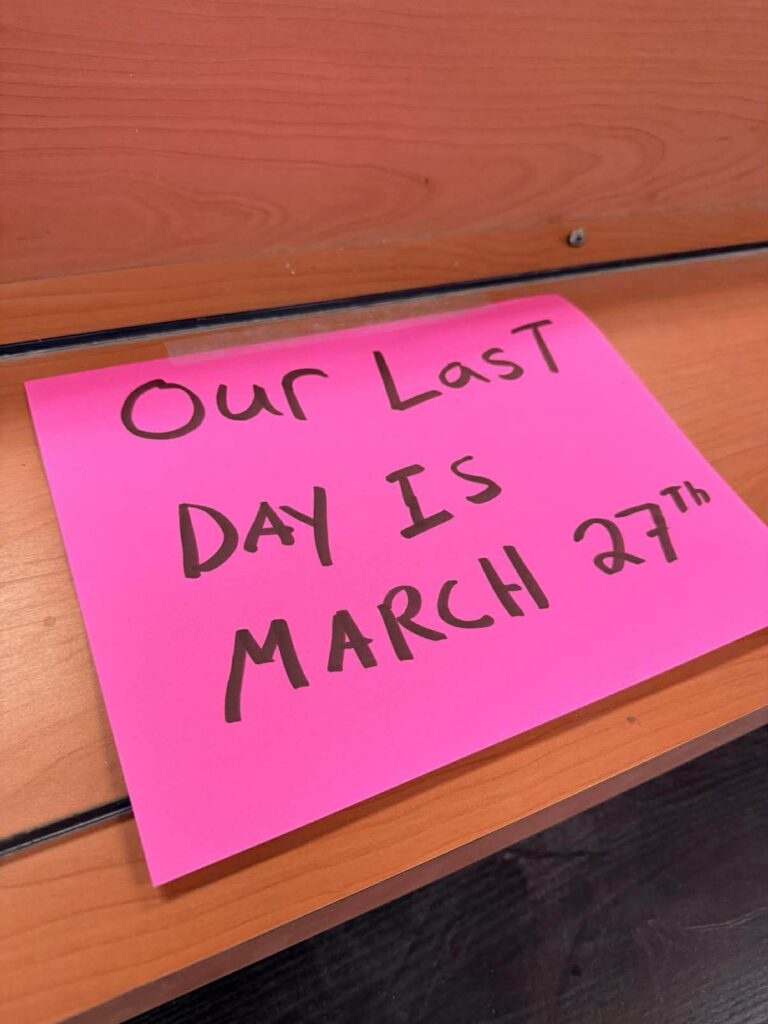
My experience with cardiologists has not been stellar. The first specialist said, “well afib is an inconvenience”. I suspect she never had an afib episode and experienced the discomfort and anxiety it creates. My second cardiologist, whom I met in late May via Zoom, spoke to me 5-10 minutes, agreed I was a candidate for ablation and said, “see you in a year”. A year. When I subsequently called the Heart Institute to inquire about the scheduling of the pre-op tests, I was told these were scheduled for December 2026, 18 months away. Discouraged and upset with the idea of waiting another 18-24 months before treatment, I went down a very deep rabbit hole.
After a couple days of feeling sorry for myself, I decided I needed to take back my power and to be intentional regarding my self-care and what I was attracting. I wrote down the following: I am attracting all that is in the highest good for achieving a healthy, happy heart. I embarked on a self-care plan that included twice weekly energy work with my chiropractor, bi-monthly massage and acupressure treatment. All of these plus a ritual of meditation and breath work, helped immensely. I began research options for treatment, across Canada. I found private Cardiac Care was available in three provinces but none offered cardiac ablation. I researched afib, learned about the condition, the risks and self-care.
One day, flipping through the most recent Zoomer magazine I came across an ad which stated ‘Why Canadians Travel to Swiss Ablation for Life-Saving Heart Care’. While I initially dismissed the ad, I later shared it with Jim. His response, “What are you waiting for?” Remember that intention?
Long story short, I reached out to them, received a response, sent them my medical records, had a lengthy Zoom call with Professor Sacha Salzberg (where I learned more about my condition than from any of my specialists over the last 7+ years), discussed with Jim and booked a trip to Zurich. On October 7th I met Dr. Salzberg in person. With Jim at my side, had all the necessary testing, education, had a clinic tour and was introduced to the staff. On October 8th I had the Cardiac Ablation procedure with Dr. Zerm, a physician with 30 years’ experience in ablation and recovered in the clinic for the day. October 9th, repeat testing.
In contrast to the Canadian approach to care, the European model believes in early aggressive treatment of afib, preventing the complications that arise in the Canadian “watch and wait” approach. We can all agree that prevention is a better alternative than chronic illness. The Swiss team we had the pleasure of working with were, simply stated, professional, thorough, kind and caring. We returned home three days following the procedure. Today marks four weeks since this life changing experience and as expected, I am doing very well.
Initially I hesitated to share this experience recognizing that I am fortunate to have the resources to make the decision I did to access private treatment and expertise. That said, one of my colleagues reminded me that self-care is putting my ME FIRST philosophy into action. A reminder – ME FIRST is about remembering that anything you wish to change in the world around you begins within you. By sharing, I hope to model that self-care falls squarely in your hands, learning to speak up and advocate for yourself and taking actions that support your health.
Putting the Heart Back into Heart Care
Let me make a statement before I begin, I am a fan of our Canadian public health care system and I have had amazing experiences within our system in the past. I cannot say the same for the current level of cardiac care, at least in Ontario and from my experience. As I mentioned previously, my first cardiologist said I was not a candidate for ablation and that having afib was simply an inconvenience. My second cardiologist disagreed, with no specific explanation and placed me on the waiting list. No one took the time to explain afib to me, what to expect, what the long term might bring and offered minimal education. My internal medicine specialist in Cornwall did explain why I needed to be on medication but following Covid, met with me only by phone. When I asked for a referral to a cardiologist, it took over a year to get an appointment. When my first cardiologist left her practice, another year to see a second cardiologist.
The entire experience has been unsettling. And I know from speaking with others with the same condition that I am not alone. Yes, I understand wait times and the pressures on our health care system. What concerns me is the lack of education, the “watch and wait” philosophy, and the overwhelming lack of concern for the patient’s wellbeing. With 30% of the population age 70 and over experiencing afib, this is a significant issue. I have yet to decide how I want to approach this issue with the medical/cardiology community, I simply feel that it is time for someone to speak up. (Caveat, my experience is limited to the Ottawa Heart Institute and may not be the case elsewhere.)
Final Word
I am eternally grateful to the SwissAblation Team and Dr. Salzberg for assessing and treating me. My message to all of you is to be informed, practice self-care, set intentions, pay attention to what shows up and take action when you see possible solutions, even when they seem to be outside your reach or different from what you imagined. I can honestly say flying to Zurich for a week, having treatment and meeting with an amazing health care team was not what I imagined would happen when I set my intention.
Also shout out to my local health care support team Dr. Vanessa Caarter, Thorin Gault, Megan Healey and Heather Pasco, my husband Jim who stood by my side every step of the way and my friends and family who held me in their prayers during this great adventure.
Until Next Time, Betty Healey